| http://www.ssat.com/cgi-bin/acupanc6.cgi |
| |
Surgical Articles
Thứ Năm, 11 tháng 8, 2011
Chủ Nhật, 7 tháng 8, 2011
Cecal diverticulitis mimicking acute Appendicitis: a report of 4 cases
Case report
World Journal of Emergency Surgery 2008, 3:16 doi:10.1186/1749-7922-3-16
The electronic version of this article is the complete one and can be found online at: http://www.wjes.org/content/3/1/16
© 2008 Karatepe et al; licensee BioMed Central Ltd.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
 Figure 1. A: Intraoperative view. B: Postoperative view.
Figure 1. A: Intraoperative view. B: Postoperative view.
 Figure 2. A: Case 2. B: Case 3. C: Case 4.
Figure 2. A: Case 2. B: Case 3. C: Case 4.
of colonic diverticulosis is difficult to ascertain, however it appears that about 8.5% of people in western countries are afflicted [1]. The sigmoid colon is the most common site of diverticulosis. Right-sided diverticula occur more often in younger patients than do left-sided diverticula, and are more common in people of Asian descent than in the other populations. The majority of colonic diverticula are false diverticula in which the mucosa and muscularis mucosa have herniated through the colonic wall [2]. Solitary diverticulum of the cecum is thought to be a congenital lesion arising as a sacular projection during the sixth week of embryonic development [2,3].
Most patients with right side diverticula are asymtomatic. However, diverticulitis does occur occasionally. Because patients are young and present with right lower quadrant pain, they are often thought to suffer from acute appendicitis, and the diagnosis of right-sided diverticulitis is subsequently made in the operating room. It is difficult to differentiate cecal diverticulitis from acute appendicitis. More than 70% of patients with cecal diverticulitis were operated on with a preoperative diagnosis of acute appendicitis [3]. The correct preoperative diagnosis was made in only 5.3% of 318 patients, according to the report of Wagner and Zollinger [4]. A number of reviews report that the incidence of a correct intraoperative diagnosis oscillates between 65 and 85% [4]. In all of our cases except one, the preoperative diagnosis was acute appendicitis.
Ultrasound and computer tomography (CT) have both been evaluated in the diagnosis of right-sided diverticulitis. Chou et al [5] reviewed 934 patients with clinically indeterminate right-sided abdominal pain who went on to have an abdominal ultrasound. They reported that ultrasound has demonstrated a sensitivity of 91.3%, a specificity of 99.8% and overall accuracy of 99.5% in the diagnosis of cecal diverticulitis [5]. CT scans have a sensitivity and specificity of 98% in the diagnosis of acute appendicitis, and are highly cost-effective; hence, some authors suggest its routine use for abdominal pain in the right lower quadrant, which would probably reduce surgeries and hospital stays [5,6]. Recognition of specific imaging findings enables the radiologist to make the correct diagnosis and helps in establishing the appropriate surgical or medical therapy, thus avoiding unnecessary exploration or surgery for some of these nonsurgical conditions mimicking acute appendicitis. If preoperative examination suggests cecum diverticulitis, the most important diagnostic tool is the CT. The CT findings were similar to those of left side diverticulitis, including focal pericolonic inflammation, diverticula, colonic wall thickening, thickening of the adjacent fascia, and extraluminal mass effect.
In patients with preoperative diagnosis of cecal diverticulitis without signs of peritonitis, medical treatment with antibiotics may be sufficient [6,7]. In our cases, almost all of our patients had no history of appendectomy, so appendicitis was the main clinical suspicion in these cases, which led to the operative exploration of the abdomen. An intraoperative diagnosis is difficult upon initial exploration. In addition, when the diagnosis is made intraoperatively, the surgical management of the disease is controversial. Conservative management with antibiotics has been suggested for cecal diverticulitis diagnosed intraoperatively, but most surgeons recommend resection [8,9]. In the presence of an inflammatory mass, diverticulectomy is usually impossible, and colectomy is required. A literature review of 279 cases of surgically treated cecal diverticulitis found no mortality after ileocecal resection, but a mortality rate of 1.8% after right hemicolectomy [10,11]. Fang et al. recommend wide resection, since 29% of patients undergoing only appendectomy in their study had recurrent episodes of right diverticulitis, with 12.5% of them requiring a later right hemicolectomy [11]. In all of our patients, a diverticulectomy and incidental appendectomy were performed and postoperative periods were uneventful.
In conclusion, Preoperative diagnosis of cecal diverticulitis is important in order to decide how to manage to this condition. During the surgical procedure, if the diagnosis of acute appendicitis is in doubt, further exploration should be performed. We recommend diverticulectomy as a safe and adequate treatment for cecal diverticulitis. However, if the histopathological examination of the specimen reveals the presence of colonic cancer, a right hemicolectomy can always be performed.
Cecal diverticulitis mimicking acute Appendicitis: a report of 4 cases
Oguzhan Karatepe*, Osman B Gulcicek, Gokhan Adas, Muharrem Battal, Yasar Ozdenkaya, Idris Kurtulus, Merih Altiok and Servet Karahan
- * Corresponding author: Oguzhan Karatepe drkaratepe@yahoo.com
Department of General Surgery, Okmeydaný Training and Research Hospital, Istanbul, Turkey
The electronic version of this article is the complete one and can be found online at: http://www.wjes.org/content/3/1/16
| Received: | 21 September 2007 |
| Accepted: | 21 April 2008 |
| Published: | 21 April 2008 |
© 2008 Karatepe et al; licensee BioMed Central Ltd.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Diverticulum of the cecum is a rare, benign, generally asymptomatic lesion that manifests itself only following inflammatory or hemorrhagic complications. Most patients with inflammation of a solitary diverticulum of the cecum present with abdominal pain that is indistinguishable from acute appendicitis. The optimal management of this condition is still controversial, ranging from conservative antibiotic treatment to aggressive resection. We describe four cases that presented with symptoms suggestive of appendicitis, but were found at operation to have an inflamed solitary diverticulum.Introduction
The cecum and ascending colon are infrequently involved in diverticulosis coli. The reported frequency is about 1 in 300 appendectomies [1,2]. The etiology of cecal diverticulitis remains unclear. Even more uncommon is a true solitary dýverticulum, which contains all layers of the bowel wall and is thought to be congenital in origin. Preoperative diagnosis is difficult because the symptoms and signs of cecal diverticulitis can mimic acute appendicitis. Diagnosis of cecal diverticulitis is difficult to make preoperatively and is thus mostly made intraoperatively. The operative treatment of cecal diverticulitis varies greatly in the literature. Here we report four cases of true solitary cecal diverticulitis managed with diverticulectomy and appendectomy, and discuss the disease in view of the literature.Case 1
A 32-year-old-male was referred to our emergency unit with pain in the right lower quadrant of the abdomen, vomiting, and nausea that began two days prior to admission. His body temperature was 37.8°C. The physical examination showed rebound-tenderness in the lower right quadrant of the abdomen. Laboratory tests were normal except for high white blood count levels. CT scans showed a tumor in the cecum surrounded by an inflammatory plate. During the surgical exploration, an enlarged posterolateral wall was seen at the cecum, with a normal appendix. A diverticulectomy and incidental appendectomy were performed (Figure 1A,B). The pathological study established the presence of a solitary diverticulum of the cecum with acute diverticulitis. Figure 1. A: Intraoperative view. B: Postoperative view.
Figure 1. A: Intraoperative view. B: Postoperative view. Case 2
A 26-year-old woman was referred to our hospital after suffering from abdominal pain for four days. The progressively increasing pain started from the left hypogastric region and radiated to the lower quadrants. She had mild nausea, but no vomiting and no change in bowel habits was observed. On physical examination the bowel sounds were decreased. Upon palpation there was a muscular defense in the lower quadrants and epigastric fullness. Biochemical tests were all within the normal limits and abdominal plain X-rays revealed no abnormality. Based on the clinical findings the patient was thus considered to have acute appendicitis and underwent emergency laparotomy. At surgery, the appendix was found in the normal location with a normal appearance and a 2 × 3 cm inflamed mass was found on the anterior wall of the cecum located between the tenia libera and plica ileo-cecalis (Figure 2A). A diverticulectomy and incidental appendectomy were performed. Figure 2. A: Case 2. B: Case 3. C: Case 4.
Figure 2. A: Case 2. B: Case 3. C: Case 4. Case 3
30-year-old woman presented to the Emergency Department with a pain in right lower abdomen since the day before. The pain was continuous in nature. There was no history of vomiting, fever, and no change in bowel habits. There was a history of decreased appetite and nausea. On examination, she was well oriented with a pulse rate of 90/min and BP of 120/70 mmHg. The abdomen was soft and non-distended. There was tenderness in the right iliac fossa with a positive rebound in the right iliac fossa. Bowel sounds and rectal examination were normal. Laboratory investigations revealed a Hb of 10.4 g% and total leukocyte count of 14000. Ultrasound (USG) abdomen was negative except for probe tenderness in the right iliac fossa. In view of her history and physical examination, the patient was diagnosed as having acute appendicitis and was shifted to the theatre for an appendectomy. The vermiform appendix was absolutely normal and diverticulum was found on the posterior wall of the cecum (Figure 2B). The patient underwent an appendectomy with excision of cecal diverticulum.Case 4
A 22-year-old woman was admitted to the hospital with right abdominal pain, nausea and vomiting. She mentioned that the abdominal pain had migrated to the right lower abdomen 12 hours after onset of periumbilical pain. On physical examination, she was subfebrile (37.5°C) and had right lower abdominal tenderness with physical signs of peritonitis. Bowel sounds and rectal examination were normal. The white blood count was 14200/mm3. Plain abdominal x-ray and USG findings were normal. A preoperative diagnosis of acute appendicitis was made and a laparotomy was performed through a right lower quadrant transverse incision. The patient was taken to the theatre where a standard open appendectomy was started. During the operation a suspicious mass was found in the lower ascending colon (Figure 2C). The appendix was visualized and found to be normal. A diverticulectomy was performed.Discussion
Diverticulosis is extremly common in the United States and Europe. It is estimated that half of the population older than age 50 years has colonic diverticula. The true prevalenceof colonic diverticulosis is difficult to ascertain, however it appears that about 8.5% of people in western countries are afflicted [1]. The sigmoid colon is the most common site of diverticulosis. Right-sided diverticula occur more often in younger patients than do left-sided diverticula, and are more common in people of Asian descent than in the other populations. The majority of colonic diverticula are false diverticula in which the mucosa and muscularis mucosa have herniated through the colonic wall [2]. Solitary diverticulum of the cecum is thought to be a congenital lesion arising as a sacular projection during the sixth week of embryonic development [2,3].
Most patients with right side diverticula are asymtomatic. However, diverticulitis does occur occasionally. Because patients are young and present with right lower quadrant pain, they are often thought to suffer from acute appendicitis, and the diagnosis of right-sided diverticulitis is subsequently made in the operating room. It is difficult to differentiate cecal diverticulitis from acute appendicitis. More than 70% of patients with cecal diverticulitis were operated on with a preoperative diagnosis of acute appendicitis [3]. The correct preoperative diagnosis was made in only 5.3% of 318 patients, according to the report of Wagner and Zollinger [4]. A number of reviews report that the incidence of a correct intraoperative diagnosis oscillates between 65 and 85% [4]. In all of our cases except one, the preoperative diagnosis was acute appendicitis.
Ultrasound and computer tomography (CT) have both been evaluated in the diagnosis of right-sided diverticulitis. Chou et al [5] reviewed 934 patients with clinically indeterminate right-sided abdominal pain who went on to have an abdominal ultrasound. They reported that ultrasound has demonstrated a sensitivity of 91.3%, a specificity of 99.8% and overall accuracy of 99.5% in the diagnosis of cecal diverticulitis [5]. CT scans have a sensitivity and specificity of 98% in the diagnosis of acute appendicitis, and are highly cost-effective; hence, some authors suggest its routine use for abdominal pain in the right lower quadrant, which would probably reduce surgeries and hospital stays [5,6]. Recognition of specific imaging findings enables the radiologist to make the correct diagnosis and helps in establishing the appropriate surgical or medical therapy, thus avoiding unnecessary exploration or surgery for some of these nonsurgical conditions mimicking acute appendicitis. If preoperative examination suggests cecum diverticulitis, the most important diagnostic tool is the CT. The CT findings were similar to those of left side diverticulitis, including focal pericolonic inflammation, diverticula, colonic wall thickening, thickening of the adjacent fascia, and extraluminal mass effect.
In patients with preoperative diagnosis of cecal diverticulitis without signs of peritonitis, medical treatment with antibiotics may be sufficient [6,7]. In our cases, almost all of our patients had no history of appendectomy, so appendicitis was the main clinical suspicion in these cases, which led to the operative exploration of the abdomen. An intraoperative diagnosis is difficult upon initial exploration. In addition, when the diagnosis is made intraoperatively, the surgical management of the disease is controversial. Conservative management with antibiotics has been suggested for cecal diverticulitis diagnosed intraoperatively, but most surgeons recommend resection [8,9]. In the presence of an inflammatory mass, diverticulectomy is usually impossible, and colectomy is required. A literature review of 279 cases of surgically treated cecal diverticulitis found no mortality after ileocecal resection, but a mortality rate of 1.8% after right hemicolectomy [10,11]. Fang et al. recommend wide resection, since 29% of patients undergoing only appendectomy in their study had recurrent episodes of right diverticulitis, with 12.5% of them requiring a later right hemicolectomy [11]. In all of our patients, a diverticulectomy and incidental appendectomy were performed and postoperative periods were uneventful.
In conclusion, Preoperative diagnosis of cecal diverticulitis is important in order to decide how to manage to this condition. During the surgical procedure, if the diagnosis of acute appendicitis is in doubt, further exploration should be performed. We recommend diverticulectomy as a safe and adequate treatment for cecal diverticulitis. However, if the histopathological examination of the specimen reveals the presence of colonic cancer, a right hemicolectomy can always be performed.
Acknowledgements
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.References
- Papapolychroniadis C, Kaimakis D, Fotiadis P, Karamanlis E, Stefopoulou M, Kouskouras K: Perforated diverticulum of the caecum. A difficult preoperative diagnosis. Report of 2 cases and review of the literature.
Tech Coloproctol 2004, 8:116-8. PubMed Abstract | Publisher Full Text
- Griffiths EA, Bergin FG, Henry JA, Mudawi AM: Acute inflammation of a congenital cecal diverticulum mimicking appendicitis.
Med Sci Monit 2003, 9(12):107-9. PubMed Abstract | Publisher Full Text
- Lane JS, Sarkar R, Schmit PJ, Chandler CF, Thompson JE Jr: Surgical approach to cecal diverticulitis.
J Am Coll Surg 1999, 188:629-635. PubMed Abstract | Publisher Full Text
- Wagner DE, Zollinger RW: Diverticulitis of the cecum and ascending colon.
Ann Surg 1961, 83:436-43.
- Yi-Hong Chou, Hong-Jen Chiou, Chui-Mei Tiu, Jen-Dar Chen, Chong-Chuan Hsu, Chen-Hsen Lee, Wing-Yiu Lui, Guo-Shian Hung, MS , Chun Yu: Sonography of acute right side colonic diverticulitis.
Am J Surg 2001, 181:122-127. PubMed Abstract | Publisher Full Text
- Sardi A, Gokli A, Singer JA: Diverticular disease of the cecum and ascending colon. A review of 881 cases.
Am Surg 1987, 53:41-45. PubMed Abstract
- Jang HJ, Lim HK, Lee SJ, Lee WJ, Kim EY, Kim SH: Acute diverticulitis of the cecum and ascending colon: the value of thin-section helical CT findings in excluding colonic carcinoma.
Am J Roentgenol 2000, 174(5):1397-1402. PubMed Abstract | Publisher Full Text
- Graham SM, Ballantyne GH: Cecal diverticulitis: a review of the American experience.
Dis Colon Rectum 1987, 30:821. PubMed Abstract | Publisher Full Text
- Fischer MG, Farkas AM: Diverticulitis of the cecum and ascending colon.
Dis Colon Rectum 1984, 27:454. PubMed Abstract | Publisher Full Text
- Shetgiri P, Angel L, Lebenthal A, Divino CM: Cecal diverticulitis: a case report and review of the current literature.
Int Surg 2001, 86:191-194. PubMed Abstract
- Fang JF, Chen RJ, Lin BC, Hsu YB, Kao JL, Chen MF: Aggressive resection is indicated for cecal diverticulitis.
Am J Surg 2003, 185:135-40. PubMed Abstract | Publisher Full Text
Famous Patients, Famous Operations, 2002 - Part 2: The Case of a Royal Pain in the Abdomen
Introduction
The patient was a 61-year-old, extremely obese, white male who complained of acute abdominal pain. The episode began approximately 2 weeks earlier with a mild attack of abdominal pain and intense nausea unrelieved by a laxative. After resting in bed for about a day, he was able to resume some activities, although he felt weak and was easily fatigued.- Past medical history: typhoid fever at age 30, no other serious illnesses
- Social history: smoked heavily and was a moderate-to-heavy drinker
- Family history: 2 relatives died from gastric cancer
- Physical examination: obese male in obvious distress, positive physical findings limited to the abdomen, where there was marked tenderness, especially on the right side, and a sensation of a mass in the iliac fossa
- System review: negative except for marked obesity
- Course of illness: abdominal pain persisted, becoming much more severe over the next 10 days; loss of appetite, eating only small amounts of light food; continued bouts of fever and abdominal pain; an operation was performed on the 10th day after the onset of symptoms
This famous patient was King Edward VII, son of Queen Victoria. The Queen died in 1901 and Edward, who had waited many years in line for the throne as the Prince of Wales, was to be crowned king on June 26, 1902. But about 2 weeks before this much-heralded event, Edward became ill with appendicitis -- a disease that, at the beginning of the 20th century, was only beginning to be diagnosed and had a high mortality rate.
At first, Edward adamantly refused to consider the possibility of surgery because it would mean postponing his highly anticipated coronation, and because appendectomy was not widely accepted in 1902. The King's physicians suggested that Frederick Treves, a surgeon, be called to examine the seriously ill patient. Treves, who had lectured and written about appendicitis (then called "perityphilitis") recommended an operation, but the King protested: "I have a coronation on hand." Treves replied, "It will be a funeral if you don't have the operation."[1]
Finally, the King consented and the operation, which lasted less than an hour, took place at Buckingham Palace. Treves located and drained an appendiceal abscess without removing the appendix. After the King's swift recovery, the coronation was held on August 9, 1902.
Appendicitis is no longer considered a diagnostic or surgical challenge, but at the beginning of the 20th century, little was known about the disease or its treatment. Although there had been discussion that excision of the obstructed appendix was the best way to treat the disease, delayed surgery to allow time for the formation of a walled-off abscess was believed to be the safest method. This is the course that Treves followed.
Appendicitis remains the most common reason for abdominal surgery in young adults.
Current surgical strategy focuses on early diagnosis and excision of the appendix, even if there is an associated abscess. The case fatality rate for appendicitis is about 2-3 per 1000 attacks with higher rates observed in very young and older patients. As we enter the 21st century, it is unclear why the incidence of appendicitis has decreased over the past several decades, and whether this decline might be due to a change in diet or is reflective of more accurate diagnosis. Several questions about appendicitis are frequently asked.
Is Computerized Tomography (CT) Indicated as a Diagnostic Aid?
CT scans improve diagnostic accuracy, but take time and add to the cost of care. CT scans are best employed when there is diagnostic uncertainty, such as in older patients; in geographic regions where appendicitis is infrequent; or in females, in whom appendicitis can be easily confused with gynecologic conditions. If a person such as Edward VII developed symptoms and signs of appendicitis today, it is likely that a CT scan would be ordered, not so much because of who he is, but because of his age.Figure 1 shows a CT scan from an 18-year-old female who presented with a 2-day history of mid-abdominal pain that was treated with ranitidine (Zantac). She presented to the emergency department 4 days later with sudden onset of diaphoresis, nausea, vomiting, and loose stools. The patient described a classical history of appendicitis with initial mid-epigastric pain, lasting approximately 2 days, which shifted to the right lower quadrant. At surgery, a necrotic appendix was removed. The adjacent peritoneal fluid was infected; therefore the surgical wound was left open, anticipating a delayed primary closure. The patient's clinical course was further complicated by a wound infection, which required intravenous antibiotics.
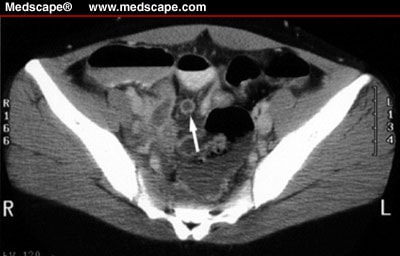
Figure 1. Computerized tomography scan from patient with acute appendicitis. Intravenous contrast-enhanced CT image of the pelvis demonstrates dilated, fluid-filled appendix (arrow). In this case, rectal contrast was not necessary to differentiate the inflamed appendix from surrounding bowel. With permission of Dr. Arun Vade, Loyola University Medical Education Network.
Is Laparoscopic Surgery Superior to the Conventional Right Lower Quadrant Open Surgical Approach?
Appendectomy can usually be performed through a small incision, allowing for a quick recovery after only a brief hospitalization. Hospitalization may be slightly shorter after laparoscopic appendectomy, but laparoscopic surgery is more expensive. If surgical reimbursement rates are low, open appendectomy is cost-effective for patients younger than 35 years of age.When Should a Surgeon Perform "Incidental" Appendectomy?
Based on the frequency of appendicitis, incidental appendectomy is indicated when feasible during performance of abdominal operations in younger patients.As a follow-up to this case, King Edward lived another 8 years without further attacks of appendicitis before dying of heart disease in 1910. Frederick Treves, the intrepid surgeon, was eventually knighted. Ironically, despite Treves' interest in and knowledge about appendicitis, his daughter died from the disease.
References
- Frederick Treves (1853-1923). The Dorset Page. Available at: http://www.thedorsetpage.com/people/Frederick_Treves.htm. Accessed April 2, 2002.
Authors and Disclosures
Albert B. Lowenfels, MD, Professor of Surgery, New York Medical College, Valhalla, New YorkMedscape General Surgery. 2002;4(1) © 2002 Medscape

Incidental appendectomy
Surg Gynecol Obstet. 1990 Jul;171(1):95-8.
Guidelines for therapeutic decision in incidental appendectomy.
Source
Department of Surgery, Southern Illinois University School of Medicine, Springfield 62794-9230.Abstract
Incidental appendectomy is contraindicated in patients whose conditions are unstable, patients previously diagnosed with Crohn's disease, patients with an inaccessible appendix, patients undergoing radiation treatment, patients who are pathologically or iatrogenically immunosuppressed and patients with vascular grafts or other foreign material. In patients ten to 30 years of age--the age group associated with a higher incidence of acute appendicitis--who are otherwise healthy, incidental appendectomy is effective in preventing morbidity and death associated with acute appendicitis. In patients 30 to 50 years of age, incidental appendectomy should be left to the discretion of the surgeon. In this age group, the physician should give special consideration to the gender of the patient and the desire for future childbirth. In patients more than 50 years of age, the incidence of acute appendicitis decreases and the risk associated with operation and prolonged anesthesia is such that an incidental appendectomy is not beneficial. In mentally handicapped patients less than 50 years of age and who are physically healthy, incidental appendectomy should be performed. An inversion technique should be used in all instances of incidental appendectomy. In otherwise clean cases in which incidental appendectomy is anticipated, prophylactic antibiotics may be of value. Patients undergoing procedures that may compromise access to the appendix in the future should undergo incidental appendectomy.Am J Surg. 2011 Apr;201(4):433-7.
Negative appendectomy: a 10-year review of a nationally representative sample.
Seetahal SA, Bolorunduro OB, Sookdeo TC, Oyetunji TA, Greene WR, Frederick W, Cornwell EE 3rd, Chang DC, Siram SM.
Source
Howard Hopkins Center for Outcomes Research, Department of Surgery, Howard University College of Medicine, Washington, DC 20060, USA. shiva_seetahal@yahoo.comAbstract
BACKGROUND:
Appendectomy remains one of the most common emergency surgical procedures encountered throughout the United States. With improvements in diagnostic techniques, the efficiency of diagnosis has increased over the years. However, the entity of negative appendectomies still poses a dilemma because these are associated with unnecessary risks and costs to both patients and institutions. This study was conducted to show current statistics and trends in negative appendectomy rates in the United States.METHODS:
A retrospective analysis was conducted using data from the National Inpatient Sample from 1998 to 2007. Adult patients (>18 y) having undergone appendectomies were identified by the appropriate International Classification of Diseases 9th revision codes. Patients with incidental appendectomy and those with appendiceal pathologies, also identified by relevant International Classification of Diseases 9th revision codes, were excluded. The remaining patients represent those who underwent an appendectomy without appendiceal disease. The patients then were stratified according to sex, women were classified further into younger (18-45 y) and older (>45 y) based on child-bearing age. The primary diagnoses subsequently were categorized by sex to identify the most common conditions mistaken for appendiceal disease in the 2 groups.RESULTS:
Between 1998 and 2007, there were 475,651 cases of appendectomy that were isolated. Of these, 56,252 were negative appendectomies (11.83%). There was a consistent decrease in the negative appendectomy rates from 14.7% in 1998 to 8.47% in 2007. Women accounted for 71.6% of cases of negative appendectomy, and men accounted for 28.4%. The mortality rate was 1.07%, men were associated with a higher rate of mortality (1.93% vs .74%; P < .001). Ovarian cyst was the most common diagnosis mistaken for appendicitis in younger women, whereas malignant disease of the ovary was the most common condition mistaken for appendiceal disease in women ages 45 and older. The most common misdiagnosis in men was diverticulitis of the colon.CONCLUSIONS:
There has been a consistent decline in the rates of negative appendectomy. This trend may be attributed to better diagnostics. Gynecologic conditions involving the ovary are the most common to be misdiagnosed as appendiceal disease in women.Copyright © 2011 Elsevier Inc. All rights reserved.
Am J Obstet Gynecol. 2011 Jan;204(1):28.e1-5.
Laparoscopic incidental appendectomy during laparoscopic surgery for ovarian endometrioma.
Source
Department of Obstetrics and Gynecology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.Abstract
OBJECTIVE:
We sought to investigate the safety and efficacy of laparoscopic incidental appendectomy during laparoscopic surgery for endometrioma.STUDY DESIGN:
We conducted a retrospective study of 356 patients undergoing laparoscopic surgery for endometrioma with appendectomy (appendectomy group, n = 172) or not (nonappendectomy group, n = 184). Primary outcome measures were operating time, hemoglobin change, hospital stay, return of bowel activity, and any complications. The secondary outcome was appendiceal histopathology.RESULTS:
There were no statistical differences between groups in operating time, postoperative changes in hemoglobin concentration, hospital stay, return of bowel activity, or complication rate. Of the 172 resected appendices, 52 had histopathologically confirmed abnormal findings including appendiceal endometriosis in 16.CONCLUSION:
Incidental appendectomy at the time of laparoscopic surgery for endometrioma does not increase operative morbidity, and it has considerable diagnostic and preventive value. However, a large prospective randomized study is needed in the future to confirm this conclusion.Copyright © 2011 Mosby, Inc. All rights reserved.
JSLS. 2009 Jul-Sep;13(3):376-83.
Incidental appendectomy during endoscopic surgery.
Source
Oak Brook Institute of Endoscopy, Rush Medical College, St. Charles, Illinois, USA.Abstract
BACKGROUND AND OBJECTIVES:
The first laparoscopic appendectomy was performed over 25 years ago, and yet controversy still exists over the open method vs. the laparoscopic approach, and whether an incidental appendectomy is warranted. This study aimed to evaluate our experience in performing a laparoscopic incidental appendectomy and to address these issues.METHODS:
A total of 772 laparoscopic appendectomies were performed and analyzed and statistically evaluated.RESULTS:
Mean age of the patients was 30.8+/-7.0 years. Mean operating time for an incidental appendectomy was 12.3+/-4.5 minutes. Most common pathology result was adhesions, and the rarest was endometriosis. Of patients with confirmed appendicitis, 75.8% did not have an initial preoperative diagnosis of appendicitis. When warranted, 103 (13.3%) patients underwent a second-look laparoscopy: 75.5% had no adhesions, 23.5% had mild adhesions, 2% had moderate adhesions. Backward elimination logistic regression revealed that endometriosis (P=0.016), endometrioma (P=0.039), pelvic or abdominal adhesions (P=0.015) were associated with a reduced likelihood of encountering appendicitis on pathology examination. The complication rate was 0.13%. Anesthesia cost was lower for an incidental appendectomy compared with an urgent one.CONCLUSION:
Laparoscopic incidental appendectomy is safe and quick to perform. Due to the complex nature of confirming the diagnosis of pelvic and abdominal pain, this study supports the routine performance of an incidental appendectomy in the female patient.Supplemental Content
- Improved outcomes for laparoscopic appendectomy compared with open appendectomy in the pediatric population. [J Laparoendosc Adv Surg Tech A. 2007] Improved outcomes for laparoscopic appendectomy compared with open appendectomy in the pediatric population.Schmelzer TM, Rana AR, Walters KC, Norton HJ, Bambini DA, Heniford BT. J Laparoendosc Adv Surg Tech A. 2007 Oct; 17(5):693-7.
- Laparoscopic appendectomy in children with perforated appendicitis. [J Laparoendosc Adv Surg Tech A. 2006] Laparoscopic appendectomy in children with perforated appendicitis.Nadler EP, Reblock KK, Qureshi FG, Hackam DJ, Gaines BA, Kane TD. J Laparoendosc Adv Surg Tech A. 2006 Apr; 16(2):159-63.
- The safety of incidental appendectomy at the time of abdominal hysterectomy. [Am J Obstet Gynecol. 2003] The safety of incidental appendectomy at the time of abdominal hysterectomy.Salom EM, Schey D, Peñalver M, Gómez-Marín O, Lambrou N, Almeida Z, Mendez L. Am J Obstet Gynecol. 2003 Dec; 189(6):1563-7; discussion 1567-8.
- Review [Laparoscopic or open appendectomy. Critical review of the literature and personal experience]. [G Chir. 2001] Review [Laparoscopic or open appendectomy. Critical review of the literature and personal experience].Cariati A, Brignole E, Tonelli E, Filippi M, Guasone F, De Negri A, Novello L, Risso C, Noceti A, Giberto M, et al. G Chir. 2001 Oct; 22(10):353-7.
- Review Appendix tumors in the era of laparoscopic appendectomy. [Surg Endosc. 2004] Review Appendix tumors in the era of laparoscopic appendectomy.Bucher P, Mathe Z, Demirag A, Morel P. Surg Endosc. 2004 Jul; 18(7):1063-6. Epub 2004 May 27.
- Related Citations Calculated set of PubMed citations closely related to the selected article(s) retrieved using a word weight algorithm. Related articles are displayed in ranked order from most to least relevant, with the “linked from” citation displayed first.
- References for this PMC Article Citation referenced in PubMed article. Only valid for PubMed citations that are also in PMC.
Aust N Z J Obstet Gynaecol. 2008 Feb;48(1):107-11.
Is incidental appendectomy necessary in women with ovarian endometrioma?
Source
Department of Obstetrics and Gynecology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, South Korea.Abstract
BACKGROUND:
Several studies reported that pathology of the appendix is frequently detected alongside endometriosis, especially with chronic pelvic pain. Furthermore, ovarian endometriosis is a marker of more extensive pelvic and intestinal disease.AIMS:
To evaluate the feasibility and efficacy of incidental appendectomy in laparoscopic surgical treatment for ovarian endometrioma.METHODS:
One hundred and six women with ovarian endometrioma underwent laparoscopic surgery including laparoscopic appendectomy. Clinicopathological data were collected and analysed.RESULTS:
The main symptoms consisted of lower abdominal pain in 51 (48.1%) women, dysmenorrhoea in 23 (21.7%), left lower quadrant pain in 6 (5.7%), right lower quadrant pain in nine (8.5%), chronic pelvic pain in five (4.7%), and others in 12 (11.3%). Only three (3.3%) of the 106 women had abnormal findings on gross inspection during laparoscopic surgery: two women with endometriotic spots on the surface of their appendixes, and one with peri-appendiceal inflammation with severe adhesions. Of the 106 resected appendixes, 37 (34.9%) had histopathologically confirmed pathology including lymphoid hyperplasia in 12 (11.3%), endometriosis in 14 (13.2%), peri-appendicitis and serositis in five (4.7%), carcinoid tumour in three (2.8%), and others in three (2.8%).CONCLUSIONS:
In all surgical treatments for ovarian endometrioma, surgeons need to preoperatively inform the patients of the fact that appendiceal pathology including endometriosis is found frequently regardless of concurrent symptoms or gross finding of the appendix. Furthermore, surgeons should take into account the possibility of appendiceal pathology during operation.Am J Obstet Gynecol. 2003 Dec;189(6):1563-7; discussion 1567-8.
The safety of incidental appendectomy at the time of abdominal hysterectomy.
Source
Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, School of Medicine, University of Miami/Jackson Memorial Hospital, 1611 NW 12th Avenue, Holtz Building East Tower Room 3003, Miami, FL 33136, USA. esalom@med.miami.eduAbstract
OBJECTIVE:
The purpose of this study was to assess the complication rates of incidental appendectomies in women who undergo benign gynecologic procedures.STUDY DESIGN:
This was a retrospective case-controlled study of patients who did (n=100 women) or did not (n=100 women) undergo incidental appendectomies at the time of an abdominal hysterectomy between June 1995 and January 2001. Information was abstracted from hospital and clinic records and a gynecologic oncology database. Data were obtained about age, body mass index, hypertension, diabetes mellitus, the number of days with nothing by mouth, the length of hospital stay, and postoperative complications (cellulitis, fever, ileus, pneumonia, thromboembolic disease). Data were analyzed with the use of two-sample t tests, Wilcoxon Rank sum tests, chi(2) tests, and multiple logistic regressions.RESULTS:
There was no difference in preoperative diagnosis or operative procedure for either group. The number of patients in the group that did have incidental appendectomy versus the group that did not have incidental appendectomy with additional procedures at the time of abdominal hysterectomy was bilateral salpingo-oophorectomy (66 vs 61 women), unilateral oophorectomy (19 vs 19 women), lysis of adhesions (9 vs 8 women), and others (12 vs 8 women). Compared with the group that did not have incidental appendectomy, the group that did have incidental appendectomy was younger (mean age+/-SD: 44+/-9.6 years vs 48+/-13.6 years, P=.02) and had a lower mean body mass index (26.1+/-6.0 kg/m(2) vs 29.8+/-8.9 kg/m(2), P=.0009). No significant differences were found between the two groups (the group that did have incidental appendectomy vs the group that did not have incidental appendectomy, respectively) with respect to the following postoperative complications: fever (40 vs 27 women), cellulitis (1 vs 2 women), wound collection (4 vs 6 women), wound dehiscence (1 vs 5 women), wound abscess (7 vs 6 women), ileus (3 vs 2 women), and urinary tract infection (4 vs 10 women). The mean length of hospital stay was significantly longer in the group that did have incidental appendectomy than in the group that did not have incidental appendectomy (3.6+/-1.52 days vs 3.1+/-1.1 days, P=.006). However, the difference was no longer significant when patients who were fed electively on the postoperative day 2 were excluded from the analysis (3.16+/-1.13 days vs 3.04+/-1.13 days, P=.507). Thirty-one percent of the histologic specimens were abnormal, with fibrous obliteration being most common, and there was one case of acute appendicitis.CONCLUSION:
An incidental appendectomy at the time of benign gynecologic procedures does not increase postoperative complication rates or length of hospital stay. The inclusion of incidental appendectomies in all abdominal hysterectomies could potentially decrease the morbidity and mortality rates because of appendicitis in elderly women.J Okla State Med Assoc. 2003 Sep;96(9):431-3.
Appendectomy at the time of cesarean section.
Source
Saint Anthony Hospital, 608 NW 9th St., Suite 1000 OKC, OK 73102, USA.Abstract
The current world literature estimates the incidence of appendicitis in pregnancy at approximately 1 case per 1500 normal deliveries. Observations of one physician and review of records from Saint Anthony Hospital in Oklahoma City have suggested potential benefit to routine examination of the appendix at the time of cesarean section and removal if it appears pathologic. The medical literature was reviewed regarding appendicitis in pregnancy and incidental or indicated appendectomy at the time of cesarean section. Many authors have described difficulties with diagnosis, as well as potential complications of appendicitis in pregnancy. Studies have confirmed the safety of performing incidental appendectomy at the time of cesarean section. The authors, therefore, propose that clinicians visualize and palpate the appendix at all cesarean sections, and remove those with evidence of inflammation or disease.Infect Dis Obstet Gynecol. 1998;6(1):30-7.
Incidental appendectomy--yes or no? A retrospective case study and review of the literature.
Source
Department of Obstetrics and Gynecology, Wake Forest University School of Medicine, Winston-Salem, NC 27157, USA.Abstract
OBJECTIVE:
A retrospective review of appendectomies performed at the University of Kansas Medical Center between January 1, 1989, and January 1, 1994, was conducted. In addition, the literature evaluating effectiveness of incidental appendectomy in preventing future operation and morbidity from appendicitis was reviewed. The results of the two reviews were analyzed to formulate guidelines for the appropriateness of performing incidental appendectomy in association with other operative procedures.METHOD:
A retrospective review of results of appendectomies performed in 460 patients at the University of Kansas Medical Center with analysis of operative findings, pathology of the removed appendix and operative complications was performed. These results were compared with those of a systematic review of the literature utilizing a Medline search relating to the subject of incidental appendix removal.RESULTS:
Two hundred sixty-one incidental appendectomies were performed in this study of 460 patients (60%). The procedure was most commonly performed with total abdominal hysterectomy (56%), followed by oophorectomy (15%) and exploratory laparotomy (11%). Morbidity was minimal at all ages. Microscopic pathology was found in 25% of the cases.CONCLUSION:
The data from the current survey and literature review support incidental removal of the appendix in the young patient (< 35 years old). In patients 35-50 years old the literature is controversial, and the patient's clinical condition and judgment of the operating surgeon should determine whether incidental appendectomy should be performed. However, routine incidental appendectomy cannot be justified in patients greater than age 50.J Am Coll Surg. 2001 Feb;192(2):182-8.
Incidental appendectomy in the era of managed care and laparoscopy.
Source
Department of Surgery, University of Rochester Medical Center, NY 14642-8410, USA.Abstract
BACKGROUND:
In a study carried out before laparoscopy or managed care, there was no cost or patient benefit for routine incidental appendectomy. With the onset oflaparoscopy, a change in indications for surgery, and increased prevalence of capitated contracts, a reanalysis of the cost-effectiveness of incidental appendectomy is warranted.STUDY DESIGN:
Financial data from 251 patients undergoing appendectomy for acute appendicitis without complication at a single institution were identified. Age-specific epidemiology data from the Centers for Disease Control, Atlanta, were applied to assess risk and cost of future appendectomy. The net cost or savings for incidental appendectomies necessary to prevent one case of acute appendectomy was determined and stratified by gender and age to the population as a whole. Further adjustment was made for the variable level of surgeon reimbursement for incidental appendectomy.RESULTS:
At 10% surgeon reimbursement, open incidental appendectomy was cost-effective in those less than 25 years of age (< 35 years of age in a capitated system). Applied to the general population, open incidental appendectomy in those less than 25 years represented savings of up to $1,100 per 10,000 population per year. A surgeon fee of greater than 50%, or the laparoscopic approach using staplers, accrued no savings in any age groups.CONCLUSIONS:
Open incidental appendectomy at low physician reimbursement is a cost-effective procedure for patients of less than 35 years of age. A decrease in equipment cost for laparoscopic approach will extend these indications.Surg Endosc. 1998 Mar;12(3):223-5.
Incidental laparoscopic appendectomy for acute right lower quadrant abdominal pain. Its time has come.
Source
Department of General Surgery and Clinical Investigation, Naval Medical Center, 34800 Bob Wilson Drive, San Diego, CA 92134-5000, USA.Abstract
BACKGROUND:
Removing the normal appendix when operating for suspected acute appendicitis is the standard of care. The use of laparoscopy should not alter this practice.METHODS:
Retrospective review of 72 patients found to have grossly normal appendices while undergoing laparoscopy for suspected appendicitis. Twenty-eight patients underwent diagnostic laparoscopy (DL) alone while 44 patients underwent diagnostic laparoscopy with incidental laparoscopic appendectomy (ILA).RESULTS:
There was no difference in length of hospitalization (DL = 44 h, ILA = 43 h, p = 0.49) or morbidity (DL = 11%, ILA = 5%, p = 0.37). One patient required appendectomy 11 days after diagnostic laparoscopy for recurrent acute right lower quadrant abdominal pain. Five percent of resected appendices (2/44) demonstrated acute inflammation upon pathologic review.CONCLUSIONS:
Laparoscopic removal of the normal appendix produces no added morbidity or increase in length of hospitalization as compared to diagnostic laparoscopy. It demonstrates cost effectiveness by preventing missed and future appendicitis. Incidental laparoscopic appendectomy is the preferred treatment option.J Laparoendosc Surg. 1992 Aug;2(4):165-6.
Incidental appendectomy during laparoscopic cholecystectomy.
Source
Department of Surgery, Staten Island University Hospital, NY 10305.Abstract
An operative experience of three patients who underwent incidental laparoscopic appendectomy during laparoscopic cholecystectomy is presented. The technique and indications are discussed. The authors conclude that incidental laparoscopic appendectomy is possible and safe with existing incisions performed in gallbladder surgery. However, well-controlled prospective studies should be performed prior to wide application of this technique.Todays OR Nurse. 1991 Dec;13(12):12-8.
Laparoscopic appendectomy incidental to gynecologic procedures.
Abstract
1. The advantages of laparoscopic appendectomy over the traditional "open" method include decreased chance of wound infection, early ambulation and resumption of normal daily activities, decreased postoperative pain, improved diagnostic accuracy, better visualization of intra-abdominal anatomy, improved cosmetic results, and avoidance of "open" appendectomy if pathology is found during routine gynecologic laparoscopic surgery. 2. Single-puncture laparoscopy has several advantages over the multiple-puncture approach, including simplicity, expediency, lower cost, avoidance of potential complications associated with multiple punctures, improved cosmetic results, and flexibility to be converted into multiple-puncture laparoscopy or laparotomyAm J Obstet Gynecol. 1991 Sep;165(3):559-64.
Incidental appendectomy during videolaseroscopy.
Source
Fertility and Endoscopy Center, Laser Endoscopy Institute of Atlanta, GA 30342.Abstract
One hundred incidental appendectomies were performed in patients undergoing operative laparoscopy (videolaseroscopy) for evaluating and treating various major diseases of the reproductive organs. Except for a fever resolving within 24 hours in one case and mild periumbilical ecchymosis, there were no intraoperative or postoperative complications. All patients were discharged within 24 hours of surgery. Average hospital stay was 14 hours. All cases have been followed up for a minimum of 8 months. We believe any risk associated with elective appendectomy as reported here is minimal and outweighed by the benefits of eliminating future emergency appendectomy, simplifying future differential diagnosis of pelvic pain and removing unsuspected abnormality found in the appendix.Surg Laparosc Endosc. 1991 Jun;1(2):116-8.
Laparoscopic incidental appendectomy.
Abstract
The benefits and risks of laparoscopic incidental appendectomy are discussed. We believe a case for laparoscopic incidental appendectomy can be made for patients undergoing diagnostic laparoscopy for lower abdominal pain in whom either no cause is found, or in whom a cause other than appendicitis is discovered. No benefit from incidental appendectomy can be shown for patients undergoing laparoscopy for other disorders.Surg Gynecol Obstet. 1990 Jul;171(1):95-8.
Guidelines for therapeutic decision in incidental appendectomy.
Source
Department of Surgery, Southern Illinois University School of Medicine, Springfield 62794-9230.Abstract
Incidental appendectomy is contraindicated in patients whose conditions are unstable, patients previously diagnosed with Crohn's disease, patients with an inaccessible appendix, patients undergoing radiation treatment, patients who are pathologically or iatrogenically immunosuppressed and patients with vascular grafts or other foreign material. In patients ten to 30 years of age--the age group associated with a higher incidence of acute appendicitis--who are otherwise healthy, incidental appendectomy is effective in preventing morbidity and death associated with acute appendicitis. In patients 30 to 50 years of age, incidental appendectomy should be left to the discretion of the surgeon. In this age group, the physician should give special consideration to the gender of the patient and the desire for future childbirth. In patients more than 50 years of age, the incidence of acute appendicitis decreases and the risk associated with operation and prolonged anesthesia is such that an incidental appendectomy is not beneficial. In mentally handicapped patients less than 50 years of age and who are physically healthy, incidental appendectomy should be performed. An inversion technique should be used in all instances of incidental appendectomy. In otherwise clean cases in which incidental appendectomy is anticipated, prophylactic antibiotics may be of value. Patients undergoing procedures that may compromise access to the appendix in the future should undergo incidental appendectomy.
Đăng ký:
Bài đăng (Atom)




